 Chuck Miller, 73, grew up in the Midwest. At just three years old, he was diagnosed with pulmonary stenosis, an obstruction of the right ventricle to the pulmonary artery.
Chuck Miller, 73, grew up in the Midwest. At just three years old, he was diagnosed with pulmonary stenosis, an obstruction of the right ventricle to the pulmonary artery.
His parents were told nothing could be done, and they should not expect their child to live past age 13 or 14.
When Chuck was about eight years old, his father packed the family up and moved to Los Angeles, where Chuck underwent one of the first pediatric open
heart surgeries in Los Angeles. For the next fifty-plus years, Chuck
lived a seemingly healthy life, until a vacation in Maui saw a TIA
(mini-stroke). Back home in Orange County, Chuck’s cardiologist
prescribed a blood thinner. The medication was effective at keeping
another stroke at bay, but brought excessive bleeding and bruising. His
cardiologist tried to slowly stop the medication, but each time, Chuck
would suffer another TIA and would need to start the blood thinner
again. This continued for 12 to 13 years with no resolution in sight.
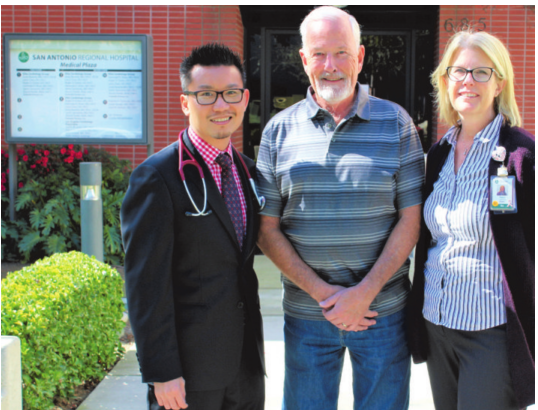
Chuck’s daughter, Alison Legendre, is a cardiac RN and the Director of Cardiac Services at San Antonio Regional Hospital.
After his fourth TIA, Alison mentioned her father’s situation to Dr. Larry Chan, DO, an interventional cardiologist at San Antonio.
Dr.
Chan suspected Chuck might have a hole in his heart which could be
causing the TIAs. He suggested that Chuck undergo a TEE (Transesophageal
Echocardiography) test available at San Antonio.
Dr. Ramesh Bansal, a specialist in TEE, performed the test, which involves placing a scope
with a camera down the esophagus to produce detailed pictures of the
heart structures and valves using high frequency sound waves.
Chuck
indeed had a hole in his heart, known as a Patient Foramen Ovale or
PFO. Dr. Chan closed the hole in Chuck’s heart through a
minimally-invasive procedure in San Antonio Regional Hospital’s cardiac
catheterization lab.
The
repair was done by threading a catheter with the closure device through
a vein in the groin, and then advanced into the area of the heart with
the defect. Transcatheter structural heart repair is shown to have good
outcomes, and quick recovery for the patient.
“It
was the easiest thing I’ve ever gone through,” Chuck said. After
suffering with ministrokes and unwanted medication complications for
years, Chuck’s heart landed in good hands and his prognosis is
excellent.